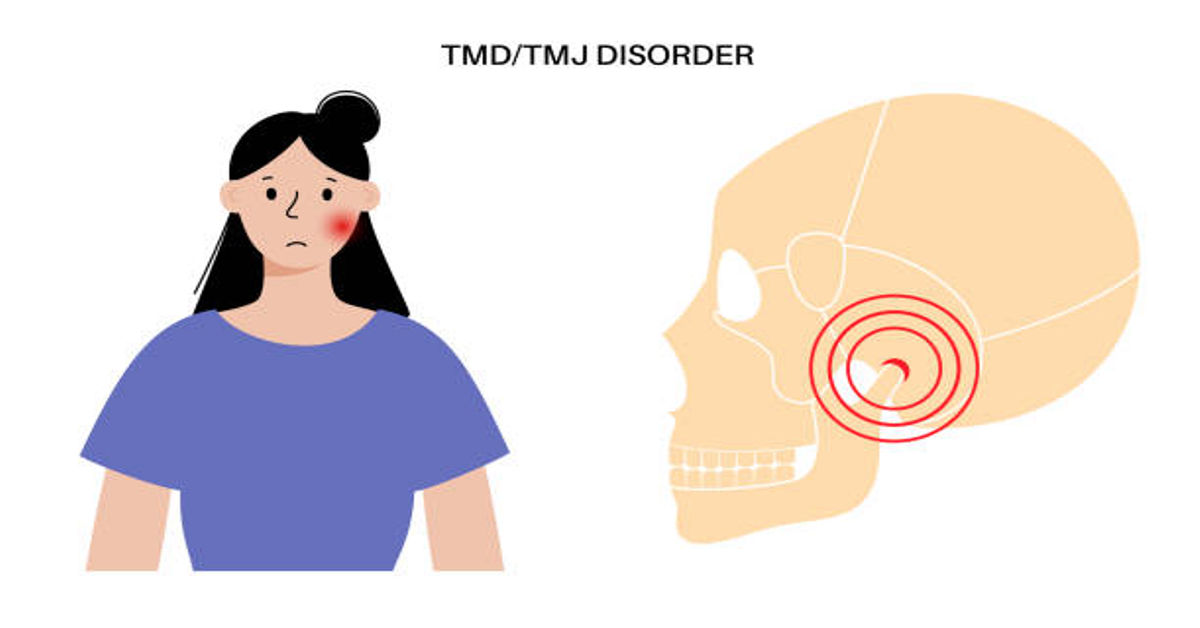
The human jaw is among the most powerful, complex, and frequently used structures in the body, participating in vital daily activities such as chewing, talking, swallowing, breathing, yawning, laughing, and facial expression. The positioned hinge that allows your lower jaw to move is called the temporomandibular joint, commonly abbreviated as TMJ Symptoms. When issues arise in this joint or in the muscles, ligaments, nerves, alignment, or movement patterns associated with it, a cluster of conditions known collectively as temporomandibular joint disorders (TMJD or TMD) may develop. One of the main reasons many individuals search for information is because TMJ-related symptoms are often confusing, overlapping, or misinterpreted, and sometimes the discomfort does not appear only near the jaw — it may radiate, spread, or masquerade as symptoms of unrelated health concerns.
This article aims to deliver a deep and holistic overview of TMJ-related symptoms from structural, neurological, muscular, and behavioral perspectives, supporting better personal awareness and informed communication with healthcare professionals. By understanding how symptoms appear, what patterns they follow, and how they interact with lifestyle, readers can become more capable of recognizing changes early, reducing escalation, and seeking timely evaluation.
Understanding the TMJ Structure and Why Symptoms Develop
The temporomandibular joint connects the mandible (lower jaw) to the temporal bone of the skull on both sides of the face, located just in front of the ears. The joint includes cartilage, ligaments, muscles, synovial fluid lubrication, and a disc-like cushion that absorbs movement impact. Unlike most body joints that move primarily in one direction, the TMJ is a hinge-sliding hybrid joint capable of forward, backward, side-to-side, and rotational movement — making it biomechanically complex. Because it is used more frequently than nearly any other joint, minor irritation, overuse, tension, or imbalance can produce noticeable symptoms.
TMJ-related problems can stem from multiple areas including joint misalignment, muscle tension, bite irregularities, parafunctional habits (unconscious repetitive actions), posture patterns, stress responses, joint inflammation, cartilage wear, or nerve sensitivity. Symptoms may be intermittent, chronic, sudden, mild, or severe, and they may affect one or both sides of the jaw.
Primary TMJ Symptoms and Sensory Patterns
TMJ symptoms may vary widely from person to person. Some individuals experience mild discomfort that fades spontaneously, while others may encounter chronic or recurring symptoms. Awareness of variations can assist in identifying early signs. Below are core symptom categories explained in comprehensive detail.
1. Jaw Pain or Discomfort
Jaw pain is one of the most recognized TMJ-related symptoms. It may manifest at rest, during chewing, speaking, yawning, or swallowing. Pain intensity may fluctuate from dull aching to sharp, localized irritation. Some individuals describe it as internal joint pain, while others feel muscular soreness near the cheeks and temples. Jaw pain may appear on one side, suggesting uneven functional tension, or on both sides when the issue is generalized or symmetrical.
2. Joint Sounds — Clicking, Popping, or Grinding
Many individuals with TMJ concerns report auditory sensations within the joint, such as clicking, popping, grinding, crackling, or crunchy textures when opening or closing the mouth. These sounds may occur because of disc displacement, ligament tension, or joint lubrication changes. Sounds are not always painful, but they may signal structural imbalance.
3. Restricted Jaw Movement or Locking Sensation
Difficulty opening or closing the mouth completely can occur, sometimes accompanied by a feeling of jaw “getting stuck” or “slipping out of place.” Jaw locking may happen when joint structures or surrounding muscles fail to move smoothly. Some individuals report morning stiffness, especially if they clench or grind their teeth during sleep.
4. Facial Muscle Soreness and Fatigue
Because the jaw muscles coordinate with facial, neck, and head muscle groups, prolonged tension can create soreness, heaviness, or fatigue in the cheeks, temples, chin, and even under the eyes. This is often compared to the feeling after chewing gum for an extended period.
Secondary and Radiating Symptoms Often Misinterpreted
One of the most confusing aspects of TMJ-related symptoms is that they frequently radiate to other regions due to shared nerve and muscle networks. The trigeminal nerve, which interacts with the TMJ, also supplies sensation to large facial segments, explaining why TMJ symptoms sometimes resemble headaches, ear problems, sinus issues, or dental pain.
Below are notable radiating symptoms:
1. Ear-Related Sensations
TMJ symptoms may resemble ear infections or inner-ear issues, presenting as:
- Earache or dull deep ear pressure
- Sensation of fullness without fluid buildup
- Tinnitus-like ringing
- Occasional dizziness or balance changes
These symptoms appear because the ear canal and TMJ share close anatomical proximity.
2. Headaches or Migraine-Like Pressure
Tension headaches around the temples, behind the eyes, or near the forehead can arise from jaw muscle strain. Individuals may feel a band-like pressure across the head, leading them to assume sinus involvement instead of jaw-related causes.
3. Neck, Upper Back, or Shoulder Discomfort
Postural tension connected to jaw clenching, forward-head posture, or bracing during stress may influence surrounding muscle chains, causing stiffness or soreness beyond the face.
Table: Common TMJ Symptoms by Category
| Category | Symptom Examples | Notes |
|---|---|---|
| Joint-Related | Clicking, popping, grinding, locking | Linked to disc or joint mechanics |
| Pain Sensation | Jaw pain, headache, ear discomfort | May radiate beyond TMJ area |
| Movement Difficulty | Limited opening, fatigue chewing | Often related to muscle strain |
| Neurological | Tingling or numb facial sensation | May stem from nerve irritation |
| Balance/Pressure | Ear fullness, dizziness | Due to anatomical proximity |
Behavioral and Lifestyle-Linked TMJ Symptom Triggers
TMJ symptoms are not always random — they may appear in response to daily habits or environmental factors. Below are common triggers that people may not recognize.
1. Jaw Clenching or Teeth Grinding
Clenching or grinding, known as bruxism, can occur consciously or subconsciously, including during sleep or stress. It places substantial pressure on the joint and surrounding muscles.
2. Stress and Emotional Tension
Stress may lead to increased jaw bracing, muscle rigidity, shallow breathing, and shoulder elevation, indirectly aggravating TMJ sensitivity.
3. Chewing Habits
Frequent gum chewing, nail biting, pen-biting, or chewing primarily on one side of the mouth can contribute to uneven joint wear.
4. Poor Posture and Device Use
Forward-head posture, often linked to prolonged device usage, may change muscle patterns in the jaw, neck, and shoulders.
5. Sleep Positioning
Sleeping face-down or on the side with pressure against the jaw may intensify joint strain.
Stages of TMJ-Related Symptom Development
TMJ symptoms may evolve gradually. The following table provides a possible awareness-oriented progression model:
| Stage | Description | Key Indicators |
|---|---|---|
| Early | Mild irregular movement | Occasional clicking or soreness |
| Developing | Noticeable tension symptoms | Headaches, fatigue, ear pressure |
| Advancing | Reduced movement range | Jaw locking, chewing discomfort |
| Chronic | Persistent discomfort patterns | Compensatory muscle involvement |
Examples of How TMJ Symptoms May Be Felt in Real Life
To help identify symptom scenarios, here are awareness-based examples:
- Feeling as if the jaw needs to “pop” to move smoothly
- Hearing clicking when eating firm textures
- Struggling to bite into large foods like apples
- Feeling tired after extended talking
- Waking up with jaw or facial soreness
Psychological and Emotional Impact of TMJ Symptoms
Persistent or uncertain symptoms can create psychological stress, including concern about dental health, neurological health, or hearing problems. Chronic discomfort may impact sleep, concentration, eating enjoyment, and social communication. When symptoms affect chewing, individuals may even modify diet texture, which can impact nutrition if prolonged.
It is helpful to remember that symptom awareness is empowering, and professional guidance can offer clarity and reassurance.
TMJ Symptom Self-Awareness Table
| Self-Check Question | Symptom Relevance |
|---|---|
| Does my jaw feel tired after talking or chewing? | Muscular fatigue |
| Do I hear sounds when opening or closing my mouth? | Joint disc involvement |
| Do I wake with soreness in my face or jaw? | Possible bruxism |
| Do headaches improve after jaw relaxation? | Muscle-related mechanism |
| Does my jaw ever feel stuck or uneven? | Movement irregularity |
Healthy Supportive Habits for Jaw Comfort (General Awareness)
The following supportive habit suggestions are not medical treatment, but general lifestyle awareness concepts:
- Use balanced chewing instead of only one side
- Maintain relaxed jaw posture with teeth slightly apart
- Avoid holding stress in facial muscles
- Monitor device-induced posture
- Practice slow breathing and calm facial expression habits
When to Consider Seeking Professional Evaluation
Professional assessment may be beneficial when symptoms:
- Persist for long periods
- Interfere with eating or speaking
- Are accompanied by noticeable jaw locking
- Cause nervous uncertainty
Multiple professionals may collaborate including dentists, physical therapists, or other qualified clinicians depending on the situation.
Conclusion
TMJ symptoms represent a broad spectrum of sensations involving the jaw joint, surrounding muscles, nerves, and head-neck structures. Understanding these symptoms from a multi-system perspective helps improve awareness, early recognition, and informed communication with health professionals. Because symptoms vary among individuals, holistic observation rather than self-diagnosis is important. When people are aware of body patterns, lifestyle habits, stress responses, and posture influences, they become better equipped to identify changes early and protect long-term joint health.
FAQs
1. Are TMJ symptoms always painful?
No, TMJ symptoms can range from painless clicking to noticeable discomfort, depending on the underlying cause and muscle involvement.
2. Can stress influence TMJ symptoms?
Yes, behavioral stress may lead to jaw muscle tension or clenching patterns that contribute to symptom development.
3. Do TMJ symptoms always require treatment?
Some mild and temporary symptoms may improve with resting habits, while persistent cases may benefit from professional evaluation.
4. Is jaw clicking always serious?
Clicking alone is not always harmful, but when paired with pain, locking, or restricted motion, evaluation is recommended.
5. Can posture affect TMJ symptoms?
Yes, head-neck posture and device-related alignment habits can influence jaw muscle tension patterns.